Liposarcoma
A fatty cancer with three distinct subtypes
Obligatory—this is not medical advice
‘So you’re saying that I’m fat’—a joke often told to me when we review the definition of a liposarcoma. Yes, they’re tumors that come from precursors of adipocytes, fat cells. It’s a simple play on words, but I always laugh. It’s part of the nature of the relationship between oncologists and their patients. We share these thoughts, observations, and puns because we’re human. It’s how we can see the light of a situation when so much here can be gloom. In all honesty, I’ve heard this joke a thousand times, from as many voices, but it still makes me smile.
What is a liposarcoma?
Liposarcomas arise from precursurs of adipocytes, and, in aggregate are approximately 25% of soft tissue sarcomas of the extremities. They can, however, arise anywhere that fat exists. We generally divide liposarcoma into 3 main subgroups. These are:
Well-differentiated/de-differentiated liposarcoma
Myxoid/Round-cell liposarcoma
Pleomorphic liposarcoma
Distinguishing the individual subtypes is highly important as there are large differences in prognosis, and treatment recommendations for each. Below is a table of what pathologists look at when they’re examining a specimen under the microscope:
As with anything, an appropriate staging workup should also be performed, which has been covered here. Most of the rest of this article will pertain to patients with advanced disease.
Well-differentiated and dedifferentiated liposarcoma (WD/DDLS)
Well and dedifferentiated liposarcomas likely exist as a spectrum of neoplasms, the first eventually becoming the next—although not always. As one might expect, outcomes are very different between the two.
Well-differentiated liposarcomas are lower grade, and, as had been expressed in prior posts is associated with improved overall survival and relapse free survival. In a review of 4300 patients in the SEER database, median age was 63 with 5 year overall survival rates of 82% and 10 year survival rates of 67%.1 Median survival was 15.8 years. Keep in mind that this is all cause survival, and not necessarily cancer specific in many instances. There is a baseline life expectancy of around 20 years for individuals who live to be 63.2
Dedifferentiated liposarcomas are usually higher grades, and are associated with lower overall survival rates. Utilizing the SEER database again, 5 year survival is 49.4% and 10 year survival is 32%. Median age was 66 and median survival was 4.9 years.
Visually, looking at each you can see the vast difference. As I might remark to patients, the second looks much ‘angrier,’ less organized, and more cancerous.
For patients in whom local therapy is expected not to improve survival or palliate symptoms, we may consider administration of systemic treatment. For patients with stable well differentiated liposarcomas, surveillance may be acceptable.
First line therapy for DDLPS is somewhat in flux, but many options could be considered reasonable and within the standard of care. These include those which have generally been trialed in other types of soft tissue sarcomas. Early phase studies have shown some promise recently, and for that reason, clinical trials should be considered early, along with referral to a sarcoma reference center. Later line trials have shown efficacy, to varying degrees, of trabectedin, and eribulin. Notably, eribulin showed a survival benefit compared to active control.3 Pazopanib should not be prescribed for patients with liposarcomas, generally speaking.
Recently studied agents include:
A larger clinical trial was published last year with selinexor for patients with DDLPS. I will explore this further, as well as perhaps some of the outcomes of that trial. 7
The SEAL trial randomized patients with advanced dedifferentiated liposarcoma 2:1 to selinexor vs placebo. Crossover was permitted. The primary endpoint of this trial was progression free survival (surrogate endpoint of growth of target lesions and death).
Here are the two points I take away:
This was an impressive undertaking and answered an important question
Numerically the placebo group lived 2.9 months longer than the treatment arm
There was a 0.7 month progression benefit for the selinexor arm (19.6 days)
Toxicity was much greater in the selinexor arm
10% of patients discontinued selinexor. Serious (eg grade 3 or 4 adverse events) happened in 38% of patients and dose reductions occurred in 36% of patients taking selinexor. Please review the manuscript for more information if you’re interested.
It does appear that a select group of patients did benefit significantly (see the portion of the the PFS curve at ~9-10 months). It is probably vital to determine the genetic and other pathophysiologic underpinnings of this population such that we can better understand who is and is not likely to benefit from Selinexor. Exploratory analyses were performed indicated CALB1 expression was associated with resistance, but hazard ratios are very wide and more data should be collected if this agent will be used in routine clinical practice.
There are ongoing studies also determining the role of cdk4/6 inhibition in patients with dedifferentiated liposarcoma (SARC041).8
Myxoid/Round-cell liposarcoma
Myxoid/round-cell liposarcomas are approximately 30% of liposarcomas, and in aggregate <5% of sarcomas (footnote 1). Reviewing the SEER database, the median age at diagnosis was 50 with a 5 year survival rate of 76%, 10 year survival of 64% and median overall survival of 17.8 years. While higher than other types of STS, keep in mind the median age is much lower for this population of patients and so a normal life expectancy would be anticipated to be longer for those individuals at baseline. One of the key factors for patients with a diagnosis of myxoid/round-cell liposarcoma is the proportion of round cells. Typical thresholds set is 5%. Patients with a diagnosis of myxoid/round cell with a round cell fraction >5% have a poorer prognosis.9
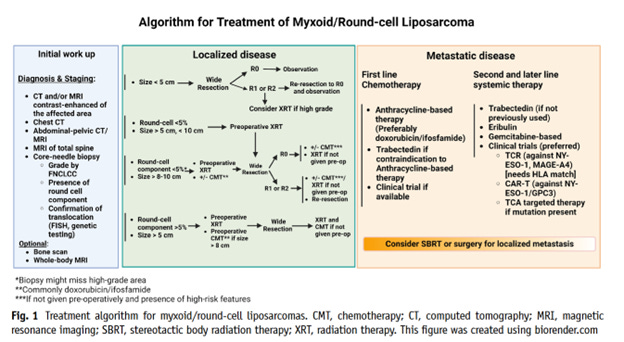
The round cell fraction may impact recommendations regarding systemic therapy with an emphasis placed on doxorubicin based chemotherapy for those with higher round cell fraction. The following treatment algorithm was provided in a recent article pertaining to the specific treatment of this neoplasm.10
Data in the neoadjuvant setting indicate that, for patients with myxoid liposarcoma and a lower round cell fraction, trabectedin may be equivalent to adriamycin, ifosfamide, and mesna (STS 1001). 11 These data again, only pertain to a select subgroup of patients, but are thought provoking.
Trabectedin may be combined with radiation for patients with myxoid liposarcoma, which is often done at our and other centers. The feasibility of this has been shown repeatedly. Careful consideration of the patient, their symptoms, and anatomy must be done. 12
Pleomorphic Liposarcoma
Pleomorphic liposarcoma is the rarest subtype of liposarcoma and is distinguished by the appearance of its lipoblasts, the precursors for adipocytes (fat cells). In a review of 1200 patients with in the SEER database, the median age for patients was 66 with a median overall survival of 5.3 years from diagnosis, 34.8% of patients were alive at 10 years (footnote #1).

Treatment for patients with pleomorphic liposarcoma follows other general sarcoma paradigms. These would involve anthracycline based treatment, consideration of gemcitabine/docetaxel, and later lines of therapy could include trabectedin, and eribulin. Importantly, patients with liposarcomas should not receive pazopanib outside of specific circumstances. The PALETTE trial did not include patients with adipocytic sarcomas (read: liposarcomas). 13
I would say that most of us sarcoma medical oncologists prefer eventual use of eribulin and trabectedin for patients with this diagnosis. Eribulin, as mentioned earlier was able to show a survival benefit against active control. The endpoint for trabectedin for patients with liposarcoma and leiomyosarcoma was progression free survival.14
Conclusions
Liposarcoma, even amongst sarcomas, is a heterogeneous group of diseases. It is important that an expert pathologist and clinical team distinguish the subtype of liposarcoma so that treatment can be catered accordingly. Patients with well differentiated, low grade liposarcomas may benefit from surgical management. Higher grade, dedifferentiated liposarcomas have many therapeutic options, but they should be selected after values based discussion and consultation with a sarcoma oncologist. Myxoid/Round cell liposarcoma is exquisitely chemo and radiosensitive and treatment is reviewed above. Pleomorphic liposarcoma hews more closely to regular soft tissue sarcoma guidelines. Pazopanib should not be used for patients with liposarcomas outside of specific circumstances.
https://pubmed.ncbi.nlm.nih.gov/32774015/
https://www.ssa.gov/oact/STATS/table4c6.html
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)01283-0/fulltext
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4991028/
https://pubmed.ncbi.nlm.nih.gov/28988646/
https://jamanetwork.com/journals/jamaoncology/article-abstract/2795419
https://pubmed.ncbi.nlm.nih.gov/35394800/
https://clinicaltrials.gov/ct2/show/NCT04967521
https://journals.lww.com/ajsp/Abstract/1996/02000/Myxoid_Round_Cell_Liposarcoma_of_the_Extremities_.5.aspx
https://pubmed.ncbi.nlm.nih.gov/36853469/
https://pubmed.ncbi.nlm.nih.gov/32077895/
https://pubmed.ncbi.nlm.nih.gov/22595799/
https://ascopubs.org/doi/10.1200/jco.2015.62.4734