Getting Started with Neoadjuvant treatment
The first step can often be the most difficult
Obligatory - This is not medical advice
What is Neoadjuvant Treatment?
When I talk to learners who work with me, we start first by defining terms. You need to comprehend the principle before you can move on to analyze or act on it.
So, what is neoadjuvant treatment? The term means treatment prior to the main therapy. Typically in oncology, and therefore the sarcoma world, this means chemotherapy or radiation prior to a surgery. The intention had historically been to improve the facility of a surgery, although we are in the process of sorting through this as a field. There are varied indications and strengths of evidence depending upon the type of cancer. There may also be differential effects between giving chemotherapy or immunotherapy before or after a surgery. A recent study with immunotherapy in patients who have stage III and IV melanoma, for instance, shows that there could be delayed relapse for immunotherapy given prior to surgery. This data will need more time to mature and further trials should be performed to disentangle other remaining questions. As a field, we are still parsing through the details.
Neoadjuvant therapy for Soft Tissue Sarcoma of the Extremity
This is about as controversial as things get in our field—and that’s saying a lot because there are many disagreements in the sarcoma universe—even between experts.
In medicine getting evidence for a practice is about doing clinical trials. This is how we answer questions. Not all questions can be answered and some compromises are often made to get at the approximate truth. In sarcoma we’ve made a lot of compromises. Let’s talk about the information we do have.
For patients with high-risk soft tissue sarcoma of the extremity there is no advantage to giving postoperative chemotherapy after 3 cycles of neoadjuvant chemotherapy with anthracycline and ifosfamide1
Great, so where do we go from here? The natural follow-up question was: are there some types of chemotherapy that are better than others? Anthracycline combined with ifosfamide is toxic, requires significant logistical consideration (sometimes given inpatient). There must be a better way, right? Members of the same group sought to answer this with the ISG-STS-1001 trial. Unfortunately, and defying the expectations perhaps of the investigators, this was not true.
For most patients with soft tissue sarcoma, anthracycline and ifosfamide is superior to other types of treatment. 2
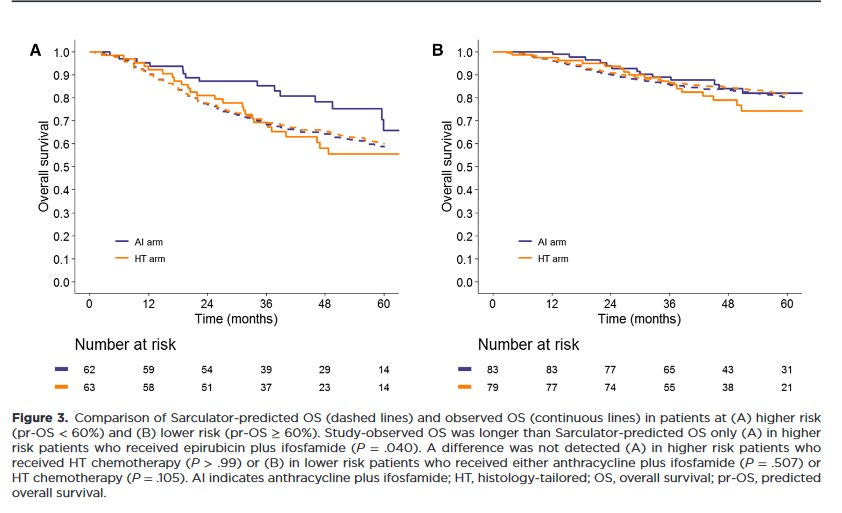
Within these, and other trials, a significant body of data was accumulated. Thousands of patients had participated in these studies. To maximize the meaning of this information, mathematical models were made to discern who was most and least likely to benefit from treatment. This culminated in an app called the Sarculator.3
It’s important to stress that this tool isn’t perfect! There are clear biases inherent in modeling on retrospective data. Nonetheless, through application to multiple trials, and over time, it has shown itself to be a decent predictor, as good as we have now, at helping establish who will and will not benefit from chemotherapy.
See the following figure4 which show, better than my words can, how the predicted overall survival (pr-OS) being less than 60% at 10 years can tell us who is most likely to benefit from chemotherapy.
Alright, I apologize for all the words here. The take home point is that not all patients need treatment. Context is king, and there are various ways to establish who is and is not likely to benefit. In future posts I’ll delve into the details of above. I know that it’s been quite the journey, and we’re just getting started.
https://www.annalsofoncology.org/article/S0923-7534(19)36553-6/fulltext
https://ascopubs.org/doi/full/10.1200/JCO.19.03289
https://www.sarculator.com/
https://acsjournals.onlinelibrary.wiley.com/doi/full/10.1002/cncr.33895



Sarculator - wow